Effects of fungal infections associated with COVID-19 in pandemic era
DOI:
https://doi.org/10.54117/gjpas.v1i2.26Keywords:
COVID-19, Fungal Infections, Invasive Fungal Infections, Antifungal drugs, Candida InfectionAbstract
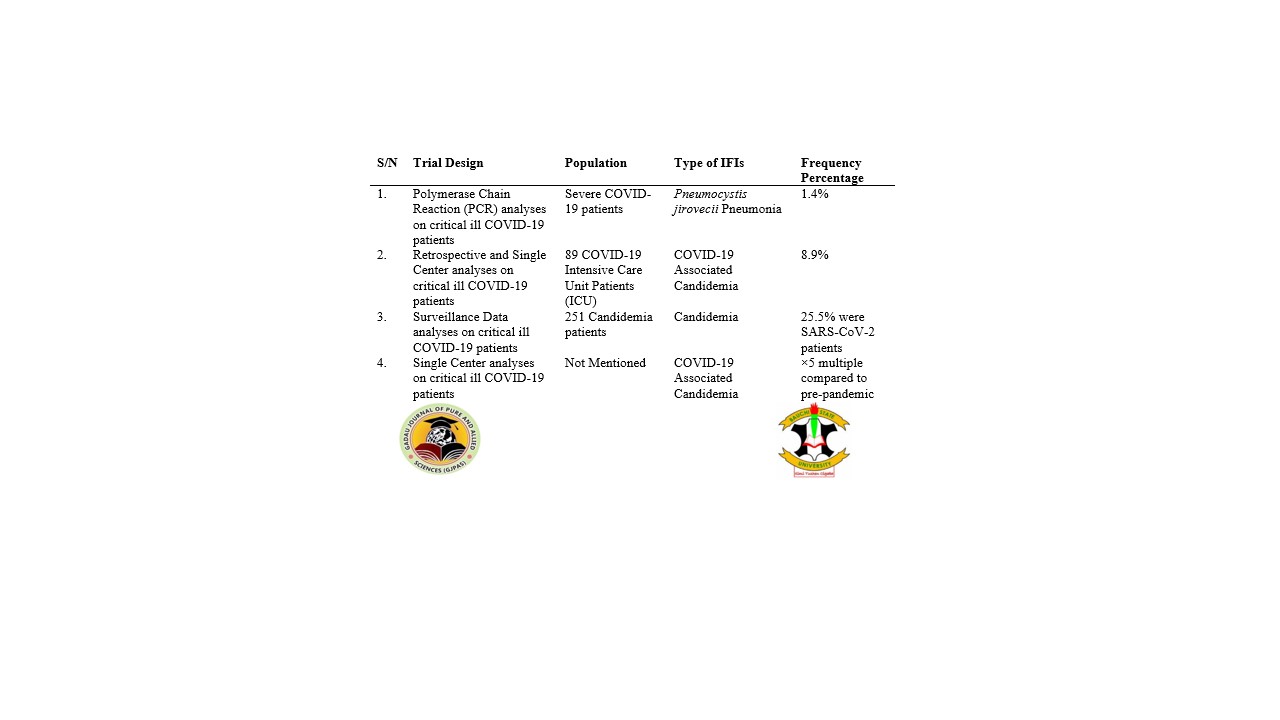
Fungal infections such as endemic mycoses, pneumocystosis, candidiasis, aspergillosis, mucormycosis and cryptococcosis associated with COVID-19 are becoming complicated in management and diagnosis of critical ill COVID-19 patients. However, mortality rates due to fungal infections are significantly high. The purpose of this study is to evaluate the effect of fungal infections associated with COVID-19 during the pandemic era. A systemic literature review was carried out to evaluate the effect of fungal infections associated with COVID-19 incidence from relevant published articles. Invasive Fungal Infections (IFIs) had the highest incidence of 26.7% from 137 intensive care unit patients screened for IFIs in 2020. Currently, drugs that are commonly used in the treatment of COVID-19 patients such as casirivimab and imdevimab, bamlanivimab and etesevimab, sotrovimab, and remdesivir had no any effects on fungal infections. In India, 53% of mortality rate which caused by 60% of Candida auris and in Brazil, 72.7% following corticosteroids use were reported. Recently, no any reports related to mortality rate due to Candida infections associated with COVID-19 in Spain and USA. Numerous current advances in management and diagnosis of these fungal infections associated with COVID-19 have not been much potentially significant. It is predicted and possible that the development of new and potent antifungal drugs, antimicrobial peptides and nanotechnology based approaches for drug delivery would help to reduce or eliminate these fungal infections associated with COVID-19 and restraint its spread across the globe.
References
Alanio, A., Delliere, S., Voicu, S., Bretagne, S. and Megarbane, B. (2020). The presence of Pneumocystis jirovecii in critically ill patients with COVID-19. Journal of Infection 82: 84–123.
Antinori, S., Bonazzetti, C., Gubertini, G., Capetti, A., Pagani, C., Morena, V., Rimoldi, S., Galimberti, L., Sarzi-Puttini, P. and Ridolfo, A.L. (2020). Tocilizumab for cytokine storm syndrome in COVID-19 pneumonia: An increased risk for candidemia? Autoimmunity Reviews 19: 102564.
Arastehfar, A., Carvalho, A., Nguyen, M.H., Hedayati, M.T., Netea, M.G., Perlin, D.S., et al. (2020). COVID-19-associated candidiasis (CAC): an underestimated complication in the absence of immunological predispositions? Journal of Fungi (Basel) 6(4): 211.
Baddley, J.W., Thompson, G.R., Chen, S.C.A., White, P.L., Johnson, M.D., Nguyen, H., Schwartz, I.S., Spec, A., Ostrosky-Zeichner, L., Jackson, B.R., et al. (2021). COVID-19-Associated Invasive Fungal Infection. Open Forum Infectious Diseases, 510.
Bardi, T., Pintado, V., Gomez-Rojo, M., Escudero-Sanchez, R., Lopez, A.A., Diez-Remesal, Y., Castro, N.M., Ruiz-Garbajosa, P. and Pestana, D. (2021). Nosocomial infections associated to COVID-19 in the intensive care unit: Clinical characteristics and outcome. European Journal of Clinical Microbiology 40: 495–502.
Basile, K., Halliday, C., Kok, J. and Chen A.C.S. (2022). Fungal infections other than invasive aspergillosis in COVID-19 patients. Journal of Fungi 8 (58): 1-17.
Benedetti, M.F., Alava, K.H., Sagardia, J., Cadena, R.C., Laplume, D., Capece, P., Posse, G., Nusblat, A.D. and Cuestas, M.L. (2020). COVID-19 associated pulmonary aspergillosis in ICU patients: Report of five cases from Argentina. Medical Mycology Case Reports 31: 24–28.
Bishburg, E., Okoh, A., Nagarakanti, S.R., Lindner, M., Migliore, C. and Patel, P. (2021). Fungemia in COVID-19 ICU patients, a single medical center experience. Journal of Medical Virology 93: 2810–2814.
Blaize, M., Mayaux, J., Luyt, C.E., Lampros, A. and Fekkar, A. (2020). COVID-19 related Respiratory Failure and Lymphopenia Do Not Seem Associated with Pneumocystosis. American Journal of Respiratory and Critical Care Medicine 202: 1734–1736.
Cafardi, J., Haas, D., Lamarre, T. and Feinberg, J. (2021). Opportunistic Fungal Infection Associated with COVID-19. In Open Forum Infectious Diseases; Oxford University Press: Oxford, UK, 8.
Campbell, L., Chen, C., Bhagat, S.S., Parker, R.A. and Ostor, A.J.K. (2011). Risk of Adverse Events Including Serious Infections in Rheumatoid Arthritis Patients Treated with Tocilizumab: A Systematic Literature Review and Meta-Analysis of Randomized Controlled Trials. Rheumatology 50: 552–562.
Chakrabarti, A. and Dhaliwal, M. (2013). Epidemiology of Mucormycosis in India. Current Fungal Infection Reports 7: 287–292.
Chen, N., Zhou, M., Dong, X., Qu, J., Gong, F., Han, Y., Qiu, Y., Wang, J., Liu, Y., Wei, Y., et al. (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 395: 507–513.
Chong, W.H., Saha, B.K., Ramani, A. and Chopra, A. (2021). State-of-the-art review of secondary pulmonary infections in patients with COVID-19 pneumonia. Infection 49: 591–605.
Chowdhary, A., Tarai, B., Singh, A. and Sharma, A. (2020). Multidrug-Resistant Candida auris Infections in Critically Ill Coronavirus Disease Patients, India, April–July 2020. Emerging Infectious Diseases 26: 2694–2696.
Choy, C.Y. and Wong, C.S. (2020). It’s not all about COVID-19: Pneumocystis pneumonia in the era of a respiratory outbreak. Journal of the International AIDS Society 23: e25533.
Cohen, S.B., Tanaka, Y., Mariette, X., Curtis, J.R., Lee, E.B., Nash, P., Winthrop, K.L., Charles-Schoeman, C., Thirunavukkarasu, K., DeMasi, R., et al. (2017). Long-Term Safety of Tofacitinib for the Treatment of Rheumatoid Arthritis up to 8.5 Years: Integrated Analysis of Data from the Global Clinical Trials. Annals of the Rheumatic Diseases 76: 1253–1262.
Dogra, S., Arora, A., Aggarwal, A., Passi, G., Sharma, A., Singh, G. and Barnwal, P.R. (2022). Mucormycosis amid COVID-19 crisis: Pathogenesis, Diagnosis and novel treatment strategies to combat the spread. Frontiers in Microbiology 12(794176): 1-27.
Fekkar, A., Lampros, A., Mayaux, J., Poignon, C., Demeret, S., Constantin, J.M., Marcelin, A. G., Monsel, A., Luyt, C.E. and Blaize, M. (2021). Occurrence of Invasive Pulmonary Fungal Infections in Patients with Severe COVID-19 Admitted to the ICU. American Journal of Respiratory and Critical Care Medicine 203: 307–317.
Fortarezza, F., Boscolo, A., Pezzuto, F., Lunardi, F., Acosta, M.J., Giraudo, C., Del Vecchio, C., Sella, N., Tiberio, I., Godi, I., et al. (2021). Proven COVID-19–associated pulmonary aspergillosis in patients with severe respiratory failure. Mycoses 64: 1223–1229.
Garcia-Vidal, C., Sanjuan, G., Moreno-Garcia, E., Puerta-Alcalde, P., Garcia-Pouton, N., Chumbita, M., Fernandez-Pittol, M., Pitart, C., Inciarte, A., Bodro, M., et al. (2021). Incidence of Co-Infections and Superinfections in Hospitalized Patients with COVID-19: A Retrospective Cohort Study. Clinical Microbiology and Infection 27: 83–88.
Ghanem, H. and Sivasubramanian, G. (2021). Cryptococcus Neoformans Meningoencephalitis in an Immunocompetent Patient after COVID-19 Infection. Case Reports in Infectious Diseases 2021: 1–3.
Gouzien, L., Cocherie, T., Eloy, O., Legriel, S., Bedos, J.P., Simon, C., Marque-Juillet, S., Ferre, A. and Bruneel, F. (2021). Invasive Aspergillosis associated with Covid-19: A word of caution. Infectious Disease Now 51: 383–386.
Heaney, A.K., Head, J.R., Broen, K., Click, K., Taylor, J., Balmes, J.R., Zelner, J. and Remais, J. V. (2021). Coccidioidomycosis and COVID-19 Co-Infection, United States, 2020. Emerging Infectious Diseases 27: 1266–1273.
Hoenigl, M., Seidel, D., Carvalho, A., Rudramurthy, S.M., Arastehfar, A., Gangneux, J.P., Nasir, N., Bonifaz, A., Araiza, J., Klimko, N., et al. (2022). The emergence of COVID-19- & associated mucormycosis: Analysis of cases from 18 countries. The Lancet Microbe 2022: 1-10.
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., Zhang, L., Fan, G., Xu, J., Gu, X., et al. (2020). Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 395: 497–506.
Jeican, I.I., Inisca, P., Gheban, D., Tabaran, F., Aluas, M., Trombitas, V., Cristea, V., Crivii, C., Junie, L.M. and Albu, S. (2021). COVID-19 and Pneumocystis jirovecii Pulmonary Coinfection-The First Case Confirmed through Autopsy. Medicina 57: 302.
Jeronimo, L.S., Esteves-Lima, R.P., Suzuki, T.Y.U., Discacciati, J.A.C. and Bhering, C.L.B. (2021). Oral candidiasis and COVID-19 in users of removable dentures: is special oral care needed? Gerontology 14: 1–6.
Kayaaslan, B., Eser, F., Kaya Kalem, A., Bilgic, Z., Asilturk, D., Hasanoglu, I., Ayhan, M., Tezer Tekce, Y., Erdem, D., Turan, S. et al. (2021). Characteristics of Candidemia in COVID-19 Patients; Increased Incidence, Earlier Occurrence and Higher Mortality Rates Compared to Non-COVID-19 Patients. Mycoses 64: 1083–1091.
KEVZARA® (Sarilumab). Full Prescribing Information (SAI-FPLR-SL-APR18a). Available online: https://Products.Sanofi.Us/ Kevzara/Kevzara.pdf (accessed on 31 March 2022).
Kremer, J., Li, Z.G., Hall, S., Fleischmann, R., Genovese, M., Martin-Mola, E., Isaacs, J.D., Gruben, D., Wallenstein, G., Krishnaswami, S., et al. (2013). Tofacitinib in Combination with Nonbiologic Disease-Modifying Antirheumatic Drugs in Patients with Active Rheumatoid Arthritis. Annals of Internal Medicine 159: 253.
Kundu, R. and Singla, N. (2022). COVID-19 and plethora of fungal infections. Current Fungal Infection Reports 16: 47-54.
Lai, C.C. and Yu, W.L. (2021). COVID-19 associated with pulmonary aspergillosis: a literature review. Journal of Microbiology, Immunology and Infection 54(1): 46–53.
Lamoth, F., Glampedakis, E., Boillat-Blanco, N., Oddo, M. and Pagani, J.L. (2020). Incidence of invasive pulmonary aspergillosis among critically ill COVID-19 patients. Clinical Microbiology and Infection 26: 1706–1708.
Lv, L., Gu, S., Jiang, H., Yan, R., Chen, Y., Chen, Y., et al. (2021). Gut mycobiota alterations in patients with COVID-19 and H1N1 infections and their associations with clinical features. Communications Biology 4(1): 480.
Marr, K.A., Platt, A., Tornheim, J.A., Zhang, S.X., Datta, K., Cardozo, C., et al. (2021). Aspergillosis complicating severe coronavirus disease. Emerging Infectious Diseases 27 (1): 18–25.
Meawed, T.E., Ahmed, S.M., Mowafy, S.M., Samir, G.M. and Anis, R.H. (2021). Bacterial and fungal ventilator associated pneumonia in critically ill COVID-19 patients during the second wave. Journal of Infection and Public Health 14: 1375–1380.
Meijer, E.F.J., Dofferhoff, A.S.M., Hoiting, O. and Meis, J.F. (2021). COVID-19-associated pulmonary aspergillosis: A prospective single-center dual case series. Mycoses 64: 457–464.
Menon, A.A., Berg, D.D., Brea, E.J., Deutsch, A.J., Kidia, K.K., Thurber, E.G., Polsky, S.B., Yeh, T., Duskin, J.A., Holliday, A.M., et al. (2020). A Case of COVID-19 and Pneumocystis Jirovecii Coinfection. American Journal of Respiratory and Critical Care Medicine 202: 136–138.
Moser, D., Biere, K., Han, B., Hoerl, M., Schelling, G., Chouker, A. and Woehrle, T. (2021). COVID-19 impairs immune response to Candida albicans. Frontiers in Immunology 12: 640644.
Mouren, D., Goyard, C., Catherinot, E., Givel, C., Chabrol, A., Tcherakian, C., Longchampt, E., Vargaftig, J., Farfour, E., Legal, A., et al. (2021). COVID-19 and Pneumocystis Jirovecii Pneumonia: Back to the Basics. Respiratory Medicine and Research 79: 100814.
Musuuza, J.S., Watson, L., Parmasad, V., Putman-Buehler, N., Christensen, L. and Safdar, N. (2021). Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: A systematic review and meta-analysis. PLoS ONE 16: e0251170.
Nucci, M., Barreiros, G., Guimaraes, L.F., Deriquehem, V.A., Castineiras, A.C., Nouer, S.A. (2020). Increased incidence of candidemia in a tertiary care hospital with the COVID-19 pandemic. Mycoses 64: 152–156.
Nucci, M., Barreiros, G., Guimaraes, L.F., Deriquehem, V.A.S., Castineiras, A.C. and Nouer, S. A. (2021). Increased incidence of candidemia in a tertiary care hospital with the COVID-19 pandemic. Mycoses 64 (2): 152–6.
Obata, R., Maeda, T., Rizk, D. and Kuno, T. (2021). Increased Secondary Infection in COVID-19 Patients Treated with Steroids in New York City. Japanese Journal of Infectious Diseases 74: 307–315.
OLUMIANT (Baricitinib). Tablets FDA Product Insert Reference ID: 4271150. Available online: https://www.Accessdata.Fda. gov/Drugsatfda_docs/Label/2018/207924s000lbl.Pdf (accessed on 31 March 2022).
Passarelli, V.C., Perosa, A.H., de Souza Luna, L.K., Conte, D.D., Nascimento, O.A., Ota-Arakaki, J. and Bellei, N. (2020). Detected SARS-CoV-2 in Ascitic Fluid Followed by Cryptococcemia: A Case Report. SN Comprehensive Clinical Medicine 2: 2414–2418.
Prestel, C., Anderson, E., Forsberg, K., Lyman, M., de Perio, M.A., Kuhar, D., Edwards, K., Rivera, M., Shugart, A., Walters, M., et al. (2021). Candida auris outbreak in a COVID-19 specialty care unit—Florida, July–August 2020. Morbidity and Mortality Weekly Report 70: 56–57.
Richardson, M. (2009). The ecology of the Zygomycetes and its impact on environmental exposure. Clinical Microbiology and Infection 15: 2–9.
Riche, C.V.W., Cassol, R. and Pasqualotto, A.C. (2020). Is the Frequency of Candidemia Increasing in COVID-19 Patients Receiving Corticosteroids? Journal of Fungi 6: 286.
Riley, T.T., Muzny, C.A., Swiatlo, E. and Legendre, D.P. (2016). Breaking the Mold. Annals Pharmacotherapy 50: 747–757.
Rovina, N., Koukaki, E., Romanou, V., Ampelioti, S., Loverdos, K., Chantziara, V., Koutsoukou, A. and Dimopoulos, G. (2022). Fungal infections in critical ill COVID-19 patients: inevitabile malum. Journal of Clinical Medicine 11 (2017): 1-22.
Rubiano, C., Tompkins, K., Sellers, S.A., Bramson, B., Eron, J., Parr, J.B. and Schranz, A.J. (2020). Pneumocystis and Severe Acute Respiratory Syndrome Coronavirus 2 Coinfection: A Case Report and Review of an Emerging Diagnostic Dilemma. Open Forum Infectious Diseases 8: 633.
Rutsaert, L., Steinfort, N., Van Hunsel, T., Bomans, P., Naesens, R., Mertes, H., Dits, H. and Van Regenmortel, N. (2020). COVID-19-associated invasive pulmonary aspergillosis. Annals of Intensive Care 10: 71.
Sanchez, G.A.M., Reinhardt, A., Ramsey, S., Wittkowski, H., Hashkes, P.J., Berkun, Y., Schalm, S., Murias, S., Dare, J.A., Brown, D., et al. (2018). JAK1/2 Inhibition with Baricitinib in the Treatment of Autoinflammatory Interferonopathies. The Journal of Clinical Investigation 128: 3041–3052.
Schiff, M.H., Kremer, J.M., Jahreis, A., Vernon, E., Isaacs, J.D. and van Vollenhoven, R.F. (2011). Integrated Safety in Tocilizumab Clinical Trials. Arthritis Research and Therapy 13: 141.
Seagle, E.E., Jackson, B.R., Lockhart, S.R., Georgacopoulos, O., Nunnally, N.S., Roland, J., Barter, D.M., Johnston, H.L., Czaja, C.A., Kayalioglu, H., et al. (2021). The Landscape of Candidemia During the Coronavirus Disease 2019 (COVID-19) Pandemic. Clinical Infectious Diseases 74: 802–811.
Segrelles-Calvo, G., de SAraujo, G.R., Llopis-Pastor, E., Carrillo, J., Hernandez-Hernandez, M., Rey, L., Melean, N.R., Escribano, I., Anton, E., Zamarro, C., et al. (2021). Candida spp. co-infection in COVID-19 patients with severe pneumonia: Prevalence study and associated risk factors. Respiratory Medicine 188: 106619.
Selarka, L., Sharma, S., Saini, D., Sharma, S., Batra, A., Waghmare, V.T., Dileep, P., Patel, S., Shah, M., Parikh, T., et al. (2021). Mucormycosis and COVID-19: An epidemic within a pandemic in India. Mycoses 64: 1253–1260.
Singh, A.K., Singh, R., Joshi, S.R. and Misra, A. (2021). Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes and Metabolic Syndrome: Clinical Research and Reviews 15: 102146.
Slavin, M., van Hal, S., Sorrell, T.C., Lee, A., Marriott, D.J., Daveson, K., et al. (2015). Invasive infections due to filamentous fungi other than aspergillus: epidemiology and determinants of mortality. Clinical Microbiology Infection 21 (490): e1–490.e10.
Stasiak, C.E.S., Cardoso, F.R., de Almeida, S.A. and Rosado-de-Castro, P.H. (2021). Incidental Finding of COVID-19 Infection after [68Ga]Ga-PSMA-11 PET/CT Imaging in a Patient with Prostate Cancer. European Journal of Nuclear Medicine and Molecular Imaging 48: 653–654.
Stuck, A.E., Minder, C.E. and Frey, F.J. (1989). Risk of Infectious Complications in Patients Taking Glucocorticosteroids. Clinical Infectious Diseases 11: 954–963.
The RECOVERY Collaborative Group. (2021). Dexamethasone in Hospitalized Patients with Covid-19. The New England Journal of Medicine 384: 693–704.
Vallabhaneni, S. and Chiller, T.M. (2016). Fungal Infections and New Biologic Therapies. Current Rheumatology Reports 18: 1–10.
Villanueva-Lozano, H., Trevino-Rangel, R.J., Gonzalez, G.M., Ramirez-Elizondo, M.T., Lara-Medrano, R., Aleman-Bocanegra, M.C., et al. (2021). Outbreak of Candida auris infection in a COVID-19 hospital in Mexico. Clinical Microbiology and Infection 27 (5): 813–6.
Wahidi, M.M., Lamb, C., Murgu, S., Musani, A., Shojaee, S., Sachdeva, A., et al. (2020). Statement on the use of bronchoscopy and respiratory specimen collection in patients with suspected or confrmed COVID-19 infection. Journal of Bronchology and Intervention Pulmonology 27 (4): e52–4.
Werthman-Ehrenreich, A. (2021). Mucormycosis with orbital compartment syndrome in a patient with COVID-19. The American Journal of Emergency Medicine 42 (264): e265–264.e268.
White, P.L., Dhillon, R., Cordey, A., Hughes, H., Faggian, F., Soni, S., Pandey, M., Whitaker, H., May, A., Morgan, M., et al. (2020). A National Strategy to Diagnose Coronavirus Disease 2019–Associated Invasive Fungal Disease in the Intensive Care Unit. Clinical Infectious Disease 73: e1634–e1644.
World Health Organization—WHO Lists Additional COVID-19 Vaccine for Emergency Use and Issues Interim Policy Recommendations. Available online: https://www.who.int/news/item/07-05-2021-who-lists-additional-covid-19-vaccine for-emergency-use-and-issues-interim-policy-recommendations (accessed on 31 March 2022).
Yang, X., Yu, Y., Xu, J., Shu, H., Xia, J., Liu, H., Wu, Y., Zhang, L., Yu, Z., Fang, M., et al. (2020). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. The Lancet Respiratory Medicine 8: 475–481.
Yusuf, E., Vonk, A., van den Akker, J.P.C., Bode, L., Sips, G.J., Rijnders, B.J.A., et al. (2021). Frequency of positive aspergillus tests in COVID-19 patients in comparison to other patients with pulmonary infections admitted to the intensive care unit. Journal of Clinical Microbiology 59 (3) e02278-e2320.
Zhang, W., Zhao, Y., Zhang, F., Wang, Q., Li, T., Liu, Z., Wang, J., Qin, Y., Zhang, X., Yan, X., et al. (2020). The Use of Anti-Inflammatory Drugs in the Treatment of People with Severe Coronavirus Disease 2019 (COVID-19): The Experience of Clinical Immunologists from China. Clinical Immunology 214: 108393.
Downloads
Published
Issue
Section
License
Copyright (c) 2022 Gadau Journal of Pure and Allied Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.