Phenotypic characterization, detection of virulence factors, and antibacterial susceptibility profile of clinical isolates of Klebsiella pneumoniae
DOI:
https://doi.org/10.54117/gjpas.v1i2.11Keywords:
Klebsiella pneumonia, Virulence factors, Baggs Albino rat, Ciprofloxacin, Siderophore, HypermucoviscityAbstract
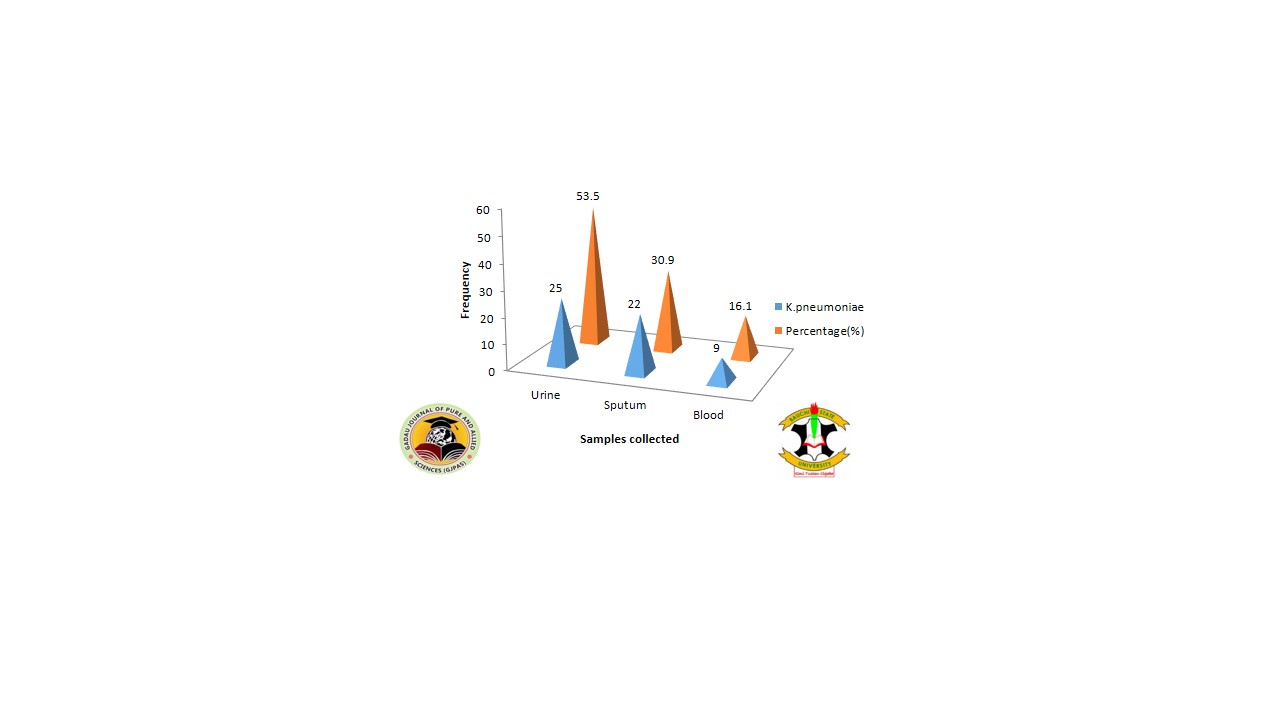
Klebsiella pneumoniae has been one of the most occurring bacteria in clinical samples causing community-acquired and nosocomial infections. It has been developing resistance to most antimicrobial agents. These have increased the pathogenicity and the chance for the evolvement of more invasive K. pneumoniae. The study was aimed at the identification and detection of Klebsiella pneumoniae from clinical samples. Some selected virulence factors were detected and the antibacterial susceptibility profile of the isolates was conducted. The incubation period, infective dose, and mortality rate of K.pneumoniae were measured using Baggs albino rats (BALB/c) strain. The isolation and identification of 56 Klebsiella pneumoniae from 223 clinical samples were made. Out of 56 K. pneumoniae isolates, all manifested mucoid phenotype, 44(78.6%) capsule antigen and 13(23.2%) Siderophore. The antimicrobial test conducted identified Zinacef 51(91.1%), Rocephin 50 (89.3%), and Ampiclox 50 (91.1%) as the most resistant. Ciprofloxacin 49 (87.5%), chloramphenicol 35(62.5%), Gentamycin 32(57.1%), and Amoxicillin 28 (50%) were the most susceptible to Klebsiella pneumoniae. The mouse lethality test shows that K. pneumoniae hypermucoviscous strain can cause 41.7% lethality and 66.7% mortality in Baggs Albino rats. Meanwhile an infection dose 105cfu/ml, 107cfu/ml and 109cfu/ml produced an incubation period of 9 days, 7days and 5days. The chi-square test shows no significant association between the isolate and the gender of the patients, but there is a significant association between the samples and isolates identified p <0.05. Likewise, the association between mucoid phenotype, capsule antigen, siderophore, and the type of infection is significant (p<0.05). It is finally concluded that K. pneumoniae is the second most prevailing bacterium causing community-acquired infection the resistant pattern recorded identified the test bacteria as a multidrug-resistant strain and manifestation of the virulent factor depends on the type and site of infection caused by the K. pneumoniae.
References
Abubakar, E. M. (2009). Antimicrobial susceptibility pattern of pathogenic bacteria causing urinary tract infections at the Specialist Hospital, Yola, Adamawa state, Nigeria. Journal of Clinical Medicine and Research, 1(1), 1–8.
Aher, T., Roy, A., and Kumar, P. (2012). Molecular detection of virulence genes associated with the pathogenicity of Klebsiella spp. isolated from the respiratory tract of apparently healthy as well as sick goats. Israel Journal of Veterinary Medicine, 67(4), 249–252. https://doi.org/10.5455/vetworld.2012.676-681
Akova. (2008). Sulbactam-containing beta-lactamase inhibitor combinations. Clinical Microbiology Infection, 14 (1), 185–8.
Alhasani, A. A. (2016). Virulence factors and antibiotic susceptibility patterns of multidrug resistance Klebsiella pneumoniae isolated from different clinical infections. African Journal of Microbiology Research, 10(22), 829-843.
Balows A. (2003). Manual of clinical microbiology 8th edition: P. R. Murray, E. J. Baron, J. H. Jorgenson, M. A. Pfaller, and R. H. Yolken, eds., ASM Press, 2003, 2113 pages, 2 vol, 2003 + subject and author indices, ISBN: 1-555810255-4, US$ 189.95. Diagnostic Microbiology and Infectious Disease, 47(4), 625–626. https://doi.org/10.1016/S0732-8893(03)00160-3.
Bartlett, J. (2013). Clinical Ocular Pharmacology (sed.). Elsevier, p.214. ISBN 9781483193915.
Bhagat, D., Sharma, P., Sirari, A., and Kumawat, K. C. (2014). Original Research Article Screening of Mesorhizobium spp . for control of Fusarium wilt in chickpea in vitro conditions Materials and Methods Procurement of cultures Isolation of Fusarium exosporium Biocontrol activities, 3(4), 923–930.
Blum, K. (2016). American Society of Microbiology. Retrieved November 25, 2016, from ASM: https://www.asm.org/index.php/mbiosphere/item/308-a-role-for-siderophores-in-klebsiella-pneumoniae-pathogenesis
BMROHP. (2012). Boston medical research occupational health program. Retrieved November 25, 2016, from Rohm: Boston Medical Research Occupational Health Program. Available at http://www.bu.edu/rohp/files/2012/08/KPC-Klebsiella.pdf.
Boyko, E. J., Fihn, S. D., Scholes, D., Abraham, L., and Monsey, B. (2005). The risk of urinary tract infection and asymptomatic bacteriuria among diabetic and nondiabetic postmenopausal women. American Journal of Epidemiology, 161(6), 557–564.
Broberg, C. A., Palacios, M., and Miller, V. L. (2014). Klebsiella: a long way to go towards understanding this enigmatic jet-setter. F1000 Prime Reports, 6(August), 64.
Carone, B., Xu, T., Murphy, K., and Marinus, M. (2014). High incidence of multiple antibiotic resistant cells in cultures of in enterohemorrhagic Escherichia coli O157: H7. Mutation research. , 759: 1–8.
Chander, A., and Shrestha, C. D. (2013). Prevalence of extended spectrum beta lactamase producing Escherichia coli and Klebsiella pneumoniae urinary isolates in a tertiary care hospital in Kathmandu, Nepal. BMC research notes, 6, 487. https://doi.org/10.1186/1756-0500-6-487.
Chen, L. F., Anderson, D. J., and Paterson, D. L. (2012). Overview of the epidemiology and the threat of Klebsiella pneumoniae carbapenemases (KPC) resistance. Infection and drug resistance, 5, 133–141. https://doi.org/10.2147/IDR.S26613.
Clinical and Laboratory Standards Institute (CLSI) (2014). Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fourth Informational Supplement. CLSI Document M100-S24, Wayne, 34(1).
Dangre-mudey, G., Tankhiwale, N. S., and Fule, R. P. (2012). Multidrug Resistance and Extended-Spectrum Beta-Lactamase Production in Klebsiella Species Isolated From Cases of Neonatal Septicaemia, Taylor and Francis 4(1), 59–62.
Hadis Amraie, P. S. (2014). Prevalence assessment of the magA gene and antimicrobial susceptibility of Klebsiella pneumonia from clinical specimens from Shahrekord, Iran. Iranian journal of microbiology IJM, Volume 6 Number 5 (October 2014) 311-316.
Hassan, A. K., Shahata, M. A., Refaie, E. M., and Ibrahim, R. S. (2014). Pathogenicity testing and antimicrobial susceptibility of Helicobacter pullorum isolate from the chicken origin. International Journal of Veterinary Science and Medicine, 2(1), 72–77.
Hussain, M. B., Hannan, A., Akhtar, N., Fayyaz, G. Q., Imran, M., Saleem, S., and Qureshi, I. A. (2015). Evaluation of the antibacterial activity of selected Pakistani honeys against multi-drug resistant Salmonella typhi. BMC complementary and alternative medicine, 15, 32. https://doi.org/10.1186/s12906-015-0549-z.
Janda, J.M. and Abbott, S.L. (2006). The Enterobacteria. ASM Press , Washington DC.
Jesmin, A. M. (2014). Study on Prevalence and Antibiotic Resistance Pattern of Klebsiella Isolated from Clinical Samples in the South East Region of Bangladesh. American Journal of Drug Discovery and Development, 4:73-79.
Karolina, I. A. (2010). Determination of Gentamicin Sulphate Composition and Related Substances in Pharmaceutical Preparations by LC with Charged Aerosol Detection. Chromatographia., 72(11-12): 1225–1229.
Li, B., Zhao, Y., Liu, C., Chen, Z., and Zhou, D. (2014). Molecular pathogenesis of Klebsiella pneumoniae. Future Microbiology, 9(9), 1071–81.
Nathisuwan, S., Burgess, D.S., Lewis, J.S. (2001). "Extended-Spectrum β-Lactamases: Epidemiology, Detection, and Treatment". Pharmacother., 21 (8): 920–928.
National Population Commission (NPC) (2006) Nigeria National Census: Population Distribution by Sex, State, LGAs and Senatorial District: 2006 Census Priority Tables (Vol. 3).
NIPA, (2016). National information program on antibiotics. Retrieved November 19, 2016, from http://www.antibiotics-info.org/cefuroxime.html: http://www.antibiotics-info.org/cefuroxime.html
Oluremi, I. A. (2011). Antibiotic susceptibility of common bacterial pathogens in urinary tract infections in a teaching hospital in Southwestern Nigeria. Afr. Journal. Microbiol. Res. , 5(22): 3658-.
Otajevewo, F. A. (2014). asymptomatic urinary tract infection occurrence among students of western delta university. World Journal of Medicine and Medical Science, Vol. 2, No, pp. 1 - 26, ISSN: 2330 - 1341.
Paterson, S. A. (2002). Community-acquired Klebsiella pneumoniae bacteremia: global differences in clinical patterns. Emerg Infect Dis, 8:160.
Pommier, L. E. (2010). DNA topoisomerases and their poisoning by anticancer and antibacterial drugs. Chem. Biol., 17 (5): 421–433. doi:10.1016/.
Prestinaci, F, Pezzotti P, Pantosti A. (2015); Antimicrobial resistance: a global multifaceted phenomenon. Pathog Glob Health. 2015;109 (7):309-18. doi: 10.1179/2047773215Y.0000000030. Epub Sep 7. PMID: 26343252; PMCID: PMC4768623.
Rice, LB, C. L. (2000). High-level expressed chromosomes encoded SHV-1 beta-lactamases and an outer membrane protein change confers resistance to ceftazidime and piperacillin-tazobactam in a clinical isolate of Klebsiella pneumonia. PUBMED, 44:362-367.
Sarathbabu, R. T. (2012). Antibiotic susceptibility pattern of Klebsiella pneumonia isolated from sputum, urine, and pus samples. J. Pharm. Biol. Sci., 1: 4-9.
Sharma, B. D., Bansal, R., and Gupta, B. (2012). Asymptomatic bacteriuria in diabetics. Journal, Indian Academy of Clinical Medicine, 13(1), 55–59.
Shigemura, T. k.-F. (2005). Pathogen occurrence and antimicrobial susceptibility of urinary tract infection cases during 20 years (1983-2002) at a single institution in Japan. Japanese Journal. Infect. Dis , 58,303-308.
Yu, V. L., Hansen, D. S., Ko, W. C., Sagnimeni, A., Klugman, K. P., von Gottberg, A., Goossens, H., Wagener, M. M., Benedi, V. J., and International Klebseilla Study Group (2007). Virulence characteristics of Klebsiella and clinical manifestations of K. pneumoniae bloodstream infections. Emerging infectious diseases, 13(7), 986–993. https://doi.org/10.3201/eid1307.070187.
Zhu, J., Wang, T., Chen, L., Du, H. (2021) Virulence Factors in Hypervirulent Klebsiella pneumoniae. Front Microbiol. Apr 8; 12: 642484. doi: 10.3389/fmicb.2021.642484. PMID: 33897652; PMCID: PMC8060575.
Downloads
Published
Issue
Section
License
Copyright (c) 2022 Gadau Journal of Pure and Allied Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.